Complicated UTIs
All UTIs, which are not defined as uncomplicated Meaning in a narrower sense UTIs in a patient with an increased chance of a complicated course:
I.e. all men, pregnant women, patients with relevant anatomical or functional abnormalities of the urinary tract, indwelling urinary catheters, renal diseases, and/or with other concomitant immunocompromising diseases for Example, diabetes.
RISK FACTORS FOR RECURRENT UTI
Age-related associations of rUTI in women
Young and pre-menopausal women
- Sexual intercourse
- Use of spermicide
- A new sexual partner
- A mother with a history of UTI
- History of UTI during childhood
Post-menopausal and elderly women
- History of UTI before menopause
- Urinary incontinence
- Atrophic vaginitis due to oestrogen deficiency
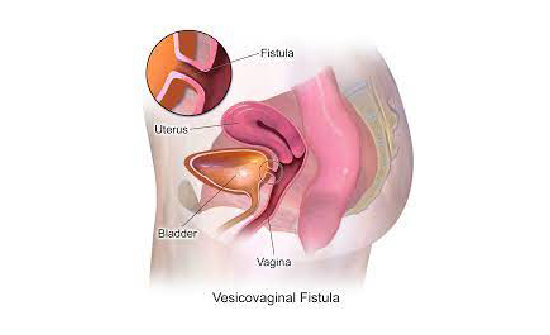
- Cystocele
- Increased post-void urine volume
- Urine catheterisation and functional status deterioration in elderly institutionalised women
Diagnostic evaluation
Clinical diagnosis of each UTI episode is supported by symptoms of dysuria, frequency, urgency, hematuria, back pain, self-diagnosis of UTI, nocturia, costovertebral tenderness and the absence of vaginal discharge or irritation.
Diagnosis of rUTI should be confirmed by urine culture.
An extensive routine workup including cystoscopy, imaging, etc. is not routinely recommended However, it should be performed without delay in atypical cases, for example,if renal calculi, outflow obstruction, interstitial cystitis or urothelial cancer is suspected.
Disease management and follow-up
Prevention of routes includes counselling regarding avoidance of risk factors, non-antimicrobial measures and Antimicrobial prophylaxis.
Any urological risk factor must be identified and treated. Significant residual urine should be treated optimally, including by CIC whenever required.
Behavioural modifications
A number of behavioural and personal hygiene measures like reduced fluid intake, habitual and post-coital delayed urination, wiping from front to back after defecation, douching and wearing occlusive underwear have Been suggested to decrease the risk of rUTI.
Non-antimicrobial prophylaxis
There are many non-antimicrobial measures recommended for rUTIs but only a few are supported by well designed studies like cranberry juice extract, D-Mannose.
Hormonal replacement
In post-menopausal women vaginal oestrogen replacement, but not oral oestrogen, showed a trend towards
Preventing rUTI.
Antimicrobials for preventing rUTI
Antimicrobials may be given as continuous low-dose prophylaxis for longer periods (three to six months), or as post-coital prophylaxis, as both regimens reduce the rate of rUTI. It should start when behavioural modifications and non-antimicrobial measures have been unsuccessful.


 '
'