Kidney Transplant Procedure & Test
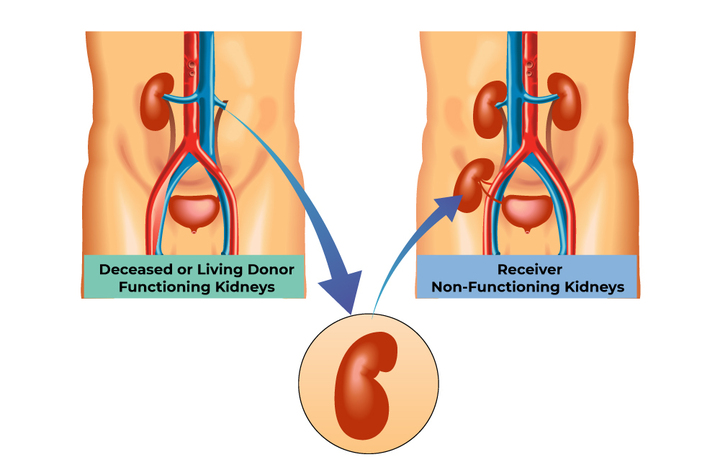
As discussed earlier, kidney transplant procedures and
testing can be divided into live and diseased donor transplantation. Live
transplantation involves the workup of the donor and recipient. The donor is
a healthy person who is subjected to donor nephrectomy as they donate to
their loved one. Donor workup should be extensive and exhaustive as any
undue harm to a donor is ethically incorrect.
In our center, the donor evaluation is done in three stages. The first stage
is a master health checkup where not only the donor's kidneys but also their
cardiac condition, pulmonary risks, blood investigations,
ultrasound-abdomen, whole GI system, and nerves are evaluated in detail.
The second stage includes renal angio dopplers, renal split function with
DTPA, and clearances from other departments including gynecology, dental,
and gastroenterology as required. These tests include a nuclear scan called
DTPA scan,
which provides split function information for each kidney
individually. This assesses the donor's risk of kidney disease. If the DTPA
scan shows unequal or low GFR, which is the function of the kidney, the
donor is rejected from donation due to the risk of further kidney disease.
The last test is the compatibility for transplantation, which is called HLA.
HLA testing includes genetic assessment for related donors and what is
called a cross-match. The following are some common kidney transplant tests:
1. Chest x-ray A chest X-ray is typically performed as part of the
kidney
transplant evaluation process to assess the donor's cardiac and pulmonary
condition.
2. Renal Nuclear Scan Renal nuclear scan, specifically DTPA scan,
is
used to provide
detailed information about the split function of each kidney individually,
helping evaluate the donor's risk of kidney disease.
3. Kidney Transplant Ultrasound With Doppler Kidney transplant
ultrasound with Doppler is conducted to assess the
anatomy and blood flow in the kidneys, aiding in the evaluation of the
suitability for transplantation.
4. Kidney Biopsy
Kidney biopsy may be performed in certain cases to obtain a tissue
sample for microscopic examination, providing valuable insights into the donor's
kidney health and potential suitability for transplantation.
5. CT Scans and MRI CT scans and MRI (magnetic resonance imaging)
may
be utilized to
gather more detailed information about the kidneys, surrounding structures, and
potential abnormalities prior to the kidney transplant procedure.
6. Blood group (ABO) incompatible Kidney Transplantation
Blood group (ABO) incompatible kidney transplantation refers to the
transplantation of a kidney from a donor with a different blood group than the
recipient, requiring additional measures such as desensitization protocols to
prevent rejection and ensure successful transplantation.